Probiotics for Allergies
Allergy season happens every year. With the spring sunshine, comes a certain amount of misery to sufferers across the Western Hemisphere every year. However, with mounting evidence linking gut health with allergies, we might have the answer to all of your allergy woes!

To find out more about allergies and the role that our gut bacteria can have in the development of allergies please read on, or if you are short of time and have a particular aspect you want to know more about, you can use the following headings to jump straight to it.
- What is an allergy?
- Types of allergies
- Allergy symptoms
- How do allergies develop?
- Can you grow out of an allergy?
- Do probiotics help allergies?
- Best probiotic strains for allergies?
- Summary
What is an allergy?
The definition of an allergy is the reaction of the body to a specific food or substance1 but what exactly does this mean? What type of reactions can we expect to see?
We know that allergies can take many different forms, encompassing reactions ranging from mild to dangerous anaphylactic reactions. I think most of us are familiar with one of the most well known food allergens, nuts, and especially peanuts. There has also been the introduction of legislation in the USA to inform customers of the presence of 8 of the most serious food allergens.

The reason for this is that a true allergy involves the immune system, and in particular a specific immunoglobulin called IgE (a type of antibody), which is implicated in anaphylaxis.
For some sufferers, allergies are an invisible and sometimes life-threatening consideration which can dominate their daily lives.
Types of allergies
Food allergies, we have already mentioned the 8 common allergens that have to be listed on ingredients and menus in the USA – milk, tree nuts, eggs, fish, shellfish, peanuts, wheat and soybeans. But there are other types of allergies that you can suffer from.
These include hay fever which is an allergy to grass and tree pollen, pets which is often a reaction to their fur or skin, insect bites/stings, latex, some medications, chemicals – including hair dyes which is why you have to do a patch test before getting your hair coloured, and even mould.
Most of these allergens are generally harmless to people who are not allergic to them. Many people are confused by the difference between a food intolerance and a food allergy. The primary difference is that whilst food intolerances can be very unpleasant, food allergies can be life-threatening.
A food allergy generally shows up as an immediate swelling of the face and airways and is an urgent condition requiring medical attention, brought on by exposure to only a small amount of the trigger substance or food.
However, an intolerance is seen as a more gradual response, generally manifesting as uncomfortable digestive symptoms, and is usually only brought on following exposure to a significant amount of the trigger 'substance'.
Allergy symptoms
Some of the most common symptoms of allergies are sneezing, coughing and itchy eyes which can be exhausting and really affect sufferer’s daily lives, influencing their daily decision-making. A trip to the park for a picnic is not so appealing if you will be constantly sneezing and rubbing your eyes.
For others their allergies can have symptoms that are much more serious, and can be life threatening and include2 skin rashes, swollen face, mouth and throat, shortness of breath and difficulty swallowing. This is an IgE response and is a rapid response to exposure to an allergen. If you suffer from an IgE allergic response you have to avoid the allergen completely.
You can also suffer from a non-IgE response which is a slower reaction and symptoms can include digestive symptoms such as diarrhoea, stomach cramps and skin conditions such as eczema. A good example of this is gluten intolerance. Sufferers from this can experience a wide array of symptoms including digestive discomfort, aching joints and lethargy. It can be quite debilitating but what causes these allergies to develop?
How do allergies develop?
The reason why we develop allergies is still poorly understood, but it is a subject of great concern to the medical profession as these inappropriate physical responses are a growing concern worldwide6.
The World Allergy Organization (WAO) warns that "the prevalence of allergic diseases worldwide is rising dramatically in both developed and developing countries."3
In particular, more and more children are presenting with allergenic symptoms, with the latest statistics indicating that more than 50% of children in the United Kingdom now suffer from some form of allergy. Evidence4 suggests that babies born via Caesarean section have an increased risk of developing allergies in later life. A natural vaginal birth exposes babies to bacteria from their mother as they pass down the birth canal, plays an important role in the development of the immune system and gut microbiota. You may like to read our article: Pregnancy and the Vaginal Microflora.
Additionally, babies that are not breastfed miss out on the 700 different species of bacteria that are present in breast milk. Coupled with the increased use of antibiotics for childhood illnesses such as tonsillitis and ear infections, babies often do not develop the strong colonies of beneficial flora that they need to support a strong immune system. Antibiotics administered in the first year of a child's life have been shown to increase their likelihood of developing an allergy by as much as 50%.
Certain individuals seem to be more pre-disposed towards allergy development: the medical profession terms these people ‘atopic.’ The word 'atopic' is derived from the Greek language and means something ‘out of place’ or ‘unusual’ – this predisposition to be ‘different’ appears to be genetic and can run in families.
Considering that most of our beneficial gut flora is initially passed on to us from our mothers via the birth canal during natural childbirth, this predisposition could be traced back to a family history of unbalanced gut flora. Research is beginning to suggest that supporting gut health via the use of live cultures may help to prevent so-called atopic symptoms such as eczema.
There is also the theory that allergies are a consequence of the diet, lifestyle and environment which has become common in western societies. A diet consisting of processed foods, coupled with stressful lifestyles and with no or little contact with a natural environment limits our exposure to naturally occurring bacteria, and is thought to be a major contributing factor to the rise in allergies. Scientists believe that this combination of factors may impact the diversity of our microbiome as well as our immune systems. This idea has been coined as the 'hygiene hypothesis', which we've discussed frequently here.
A study5 of 1,879 American adults has found further evidence to support the hypothesis. Researchers from the American National Institutes of Health sought to find out why an altered gut microbiota may increase the risk of developing allergies and other conditions. They analysed questionnaires from participants, which asked them to self-report their history of allergies, as well as faecal samples from each individual.
The researchers found that out of the 1,879 participants, 81.5% reported to have one or more allergies. This ranged from just 2.5% having a peanut allergy to 40.5% self-reporting a seasonal allergy such as hay fever. They compared questionnaire results with faecal sample results and found that those with allergies had less diversity in their gut bacteria. In fact, the more allergies an individual had the less diversity they observed in their gut bacteria.
Of single allergies, gut microbiota diversity was lowest in those with hay fever or peanut allergies. The scientists were able to identify that these individuals had lower levels of Clostridiales bacteria, and increased levels of Bacteroidales. The researchers concluded that gut microbiota intervention through the potential use of probiotics may help in the treatment or prevention of such allergies.
Can you grow out of an allergy?
There is some evidence that children can outgrow some food allergies but the rates of this for peanut and nut allergies are low, between 20-10%6. Other types of allergies, such as eczema, are more common in childhood and often resolve by teenage years but there can be relapses. There is a frustration among parents that this can mean that a distressing condition for their child is not taken seriously because of the belief that their child will grow out of it.7
Do Probiotics help allergies?
It isn’t immediately obvious to most people how supplementing with probiotics could help allergy sufferers. But the question is an interesting one, given that 70% of our immune cells are located in our intestinal tract, and that our resident gut microbiome not only interacts with the immune system but can help to modulate its responses - incredible!8
In theory, most beneficial bacteria could have some positive effect on immune function merely by helping to improve gut health, but the research is growing fast, and new information is being discovered all the time about the different bacterial strains and their individual potential.
Over the past few years a link has been established between lung microbiota and respiratory allergy, between skin microbiota and atopic dermatitis, and between gut microbiota and food allergy12. Additionally, more studies have shown that probiotics can intervene in food allergy based on the intestinal mucosal immune system14.
Best Probiotic strains for allergies
Lactobacillus acidophilus NCFM® the most extensively researched strain of L. acidophilus in the world - was used in a study where it was given to sufferers of allergic rhinitis caused by birch pollen.9
We also have articles that contain information about studies which assessed the effectiveness of Lactobacillus rhamnosus CGMCC against peanut allergy and Lacobacillus rhamnosus GG® against eczema and other atopic conditions10.

Healthcare practitioners can follow this link for more information: Lactobacillus rhamnosus GG®.
We all know histamine as the inflammatory substance produced by the body in a typical hay fever reaction, for which anti-histamine drugs are the most popular conventional treatment. But not so many people are aware that histamine is also present in many foods and can create a wide range of allergenic symptoms if the individual lacks the specific enzyme in the body, Diamine Oxidase (DAO), to effectively break this substance down. Low levels of DAO leave high serum levels of histamine circulating in the blood causing a variety of inflammatory symptoms.
Causes of histamine intolerance are thought to be intestinal permeability ('leaky gut') and SIBO (small intestinal bacterial overgrowth). So, in theory a high quality probiotic could be helpful in supporting gut health in those with histamine intolerance. The little research we have seen suggests that some strains may help to alleviate histamine intolerance by down regulating IgE and histamine receptors, and up-regulating anti-inflammatory agents in the intestinal wall, helping to repair damage and reduce permeability11.
For more information, healthcare practitioners can see our information page Which probiotics for histamine intolerance?
Since our gut microbiota may help to keep the gut healthy and enable us to break down and digest certain foods, those with food intolerances sometimes find that taking live cultures can help improve digestion and improve tolerance to offending foods
This would not be the same in the case of food allergies however, and trigger foods must always be avoided by allergic patients.
Healthcare practitioners may also like to read this article about live cultures and lactose intolerance: Which probiotics help lactose intolerance?
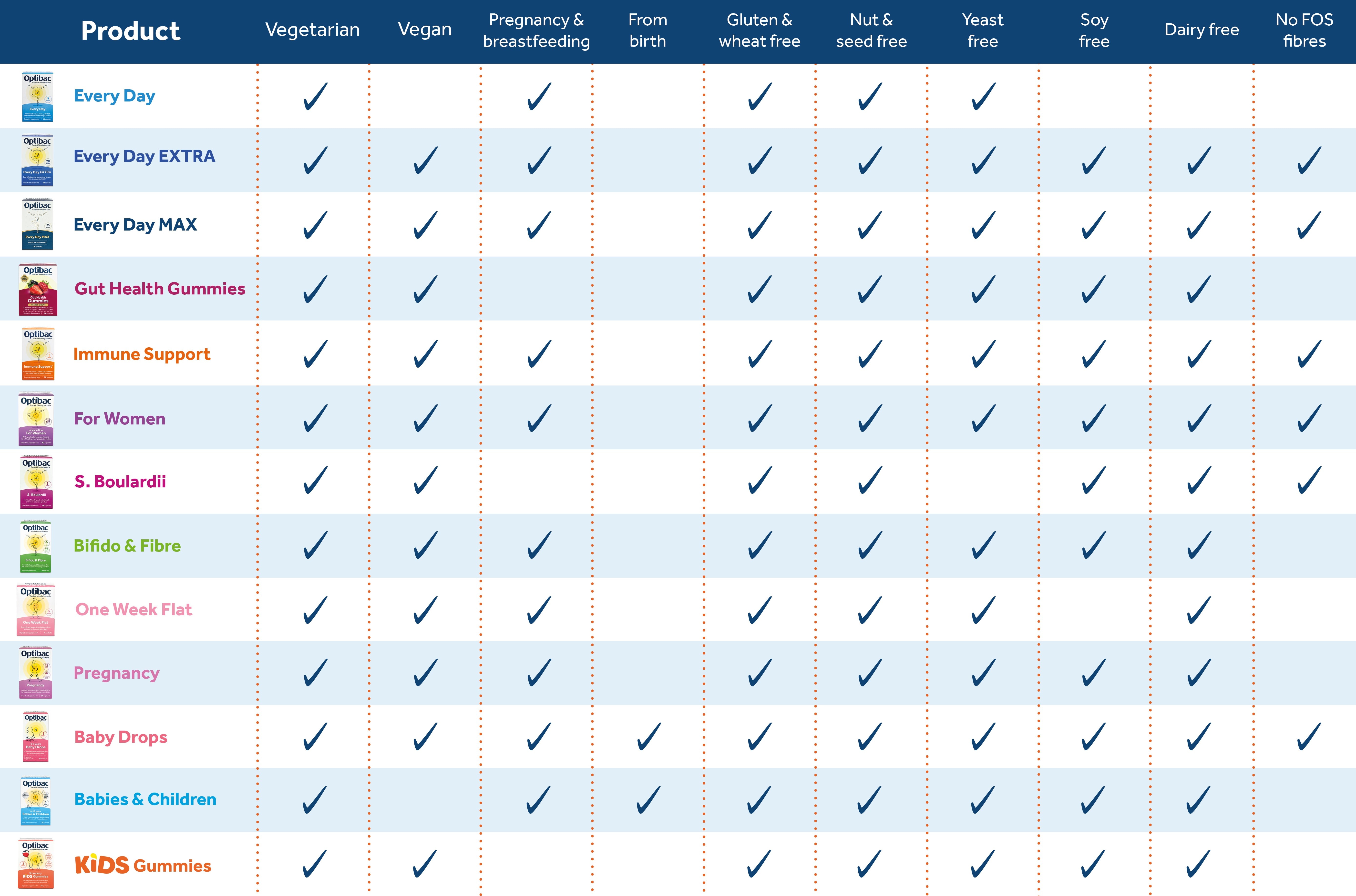
The chart below shows which of the products in our range are suitable for individuals with certain allergies.
Summary
We have learnt that allergies are a growing concern, especially amongst children, and that there are a number of theories as to why that is. There are studies that show a low diversity of gut bacteria in people with allergies. Allergies can be very serious, and in some cases, life threatening, and we now have legislation to protect sufferers from known allergens.
We have also learnt the difference between an allergy and an intolerance and can understand that both can have a debilitating effect on sufferers. Sadly, some sufferers are left feeling that they are not being taken seriously when they want help with their symptoms.
There are some strains of friendly bacteria that have been used in studies that look at allergies.
In theory, most beneficial bacteria could have some positive effect on immune function merely by helping to improve gut health, but the research is growing fast, and new information is being discovered all the time about the different bacterial strains and their individual potential. Maybe soon we will be able to share more research with you about probiotics for allergies.
If you would like to read more about how the microbiome influences the health of your baby you can read Dr. Kates in-depth article here: Baby Probiotics.
For more reading on this fascinating subject, healthcare practitioners might be interested in these other related articles:
Probiotics can help peanut allergies in kids, says new study
New study suggests probiotics can improve cow's milk allergy in infants
Could probiotics be the answer to peanut allergy?
References
- Accessed: 6/4/2022 https://www.nhs.uk/conditions/allergies/
- Accessed: 6/4/2022 https://www.nhs.uk/conditions/food-allergy/symptoms/
- Pawankar R, Canonica GW, ST Holgate ST, Lockey RF, Blaiss M. The WAO White Book on Allergy (Update. 2013)
- Henry Ford Health System. "Babies born by C-section at risk of developing allergies." ScienceDaily. ScienceDaily, 25 February 2013. <www.sciencedaily.com/releases/2013/02/130225091904.htm>.
- Xing, H. et al. (2015) Allergy association with the adult fecal microbiota: Analysis of the American Gut Project. Elsevier. Published online ahead of print, 27 November 2015.
- Outgrow an allergy Fleischer, D.M. The natural history of peanut and tree nut allergy. Curr Allergy Asthma Rep 7, 175–181 (2007). https://doi.org/10.1007/s11882-007-0018-y
- Childhood eczema - Miriam Santer, Hana Burgess, Lucy Yardley, Steven Ersser, Sue Lewis-Jones, Ingrid Muller, Catherine Hugh, Paul Little Experiences of carers managing childhood eczema and their views on its treatment: a qualitative study British Journal of General Practice 2012; 62 (597): e261-e267. DOI: 10.3399/bjgp12X636083
- Montalban-Arques A et al (2015) Selective Manipulation of the Gut Microbiota Improves Immune Status in Vertebrates, Frontiers in Immunology. Oct 9;6:512. doi: 10.3389/fimmu.2015.00512. eCollection 2015.
- Ouewhand, A.C. et al., (2009). ‘Specific probiotics alleviate allergic rhinitis during the birch pollen season’. World Journal of Gastronenterology. 15(26): 3261-3268.
- Mimi L.K. Tang, Anne-Louise Ponsonby, Francesca Orsini, Dean Tey, Marnie Robinson, Ee Lyn Su, Paul Licciardi, Wesley Burks, Susan Donath. Administration of a probiotic with peanut oral immunotherapy: A randomized trial. Journal of Allergy and Clinical Immunology, .2014.11.034
- Dev, S., Mizuguchi, H., Das, A. K., Matsushita, C., Maeyama, K., Umehara, H., ... & Fukui, H. (2008). Suppression of histamine signaling by probiotic Lac-B: a possible mechanism of its anti-allergic effect. Journal of pharmacological sciences, 107(2), 159-166
- Zubeldia-Varela E et al., (2022) Microbiome and Allergy: New Insights and Perspectives, J Investig Allergol Clin Immunol. 32(5): 327-344.
- Hui Cao et al., (2022) Adjuvant role of probiotics in allergen-specific immunotherapy, Clinical Immunology. 245: 109164.
- Gu S et al., (2023) The role of probiotics in prevention and treatment of food allergy, Food Science and Human Wellness. 12:3 681-690.
Popular Articles
View all General Health articles-
General Health03 Nov 2023
-
General Health17 Dec 2024
-
General Health06 Nov 2023